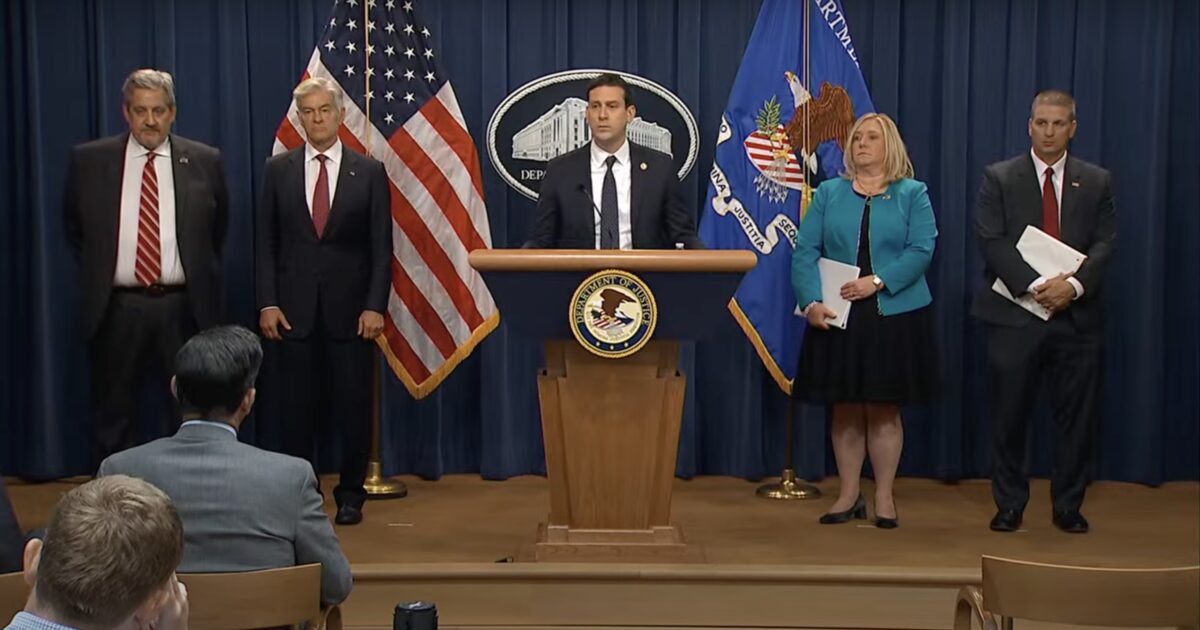
Screenshot: Fox News
The Department of Justice on Monday unveiled a record-shattering crackdown on the corrupt underbelly of America’s health care system. A jaw-dropping 324 defendants — including 96 medical professionals — have been charged in 50 federal districts and 12 states for orchestrating over $14.6 billion in intended fraud, largely targeting Medicare, Medicaid, and federal health programs meant to serve the elderly, disabled, and the poor.
The takedown, spearheaded by the DOJ’s Health Care Fraud Unit in coordination with HHS-OIG, the FBI, the DEA, and over a dozen state attorney general offices, marks the largest health care fraud bust in U.S. history.
“Today, as we announced the largest coordinated health care fraud takedown in the history of the Department of Justice, it marks a decisive moment in our fight to protect American taxpayers from fraudsters and to defend the integrity of America’s health care system,” said Matthew R. Galeotti, DOJ’s Head of the Criminal Division.
“We are announcing today charges against 324 defendants for their alleged participation in health care fraud schemes involving approximately $14.6 billion in false claims submitted to Medicare, Medicaid, and other health care programs.”
“These criminals didn’t just steal someone else’s money — they stole from you. Every fraudulent claim, every fake billing, every kickback scheme represents money taken directly from the pockets of American taxpayers who fund these essential programs through their hard work and sacrifice. And when criminals defraud these programs, they’re not just committing theft — they’re driving up our national deficit and threatening the long-term viability of health care for seniors, disabled Americans, and our most vulnerable citizens.”
WATCH:
BREAKING: The DOJ has just announced the results of the largest National Health Care Fraud Takedown in American history.
This massive operation led to criminal charges against 324 defendants—including 96 doctors, nurse practitioners, pharmacists, and other licensed medical… pic.twitter.com/gC07gzeXWG
— I Meme Therefore I Am (@ImMeme0) June 30, 2025
More from the DOJ:
Transnational Criminal Organizations
29 defendants were charged for their roles in transnational criminal organizations alleged to have submitted over $12 billion in fraudulent claims to America’s health insurance programs.
For instance, a nationwide investigation known as Operation Gold Rush resulted in the largest loss amount ever charged in a health care fraud case brought by the Department. These charges were announced in the Eastern District of New York, the Northern District of Illinois, the Central District of California, the Middle District of Florida, and the District of New Jersey against 19 defendants. Twelve of these defendants have been arrested, including four defendants who were apprehended in Estonia as a result of international cooperation with Estonian law enforcement and seven defendants who were arrested at U.S. airports and the U.S. border with Mexico, cutting off their intended escape routes as they attempted to avoid capture.
The organization allegedly used a network of foreign straw owners, including individuals sent into the United States from abroad, who, acting at the direction of others using encrypted messaging and assumed identities from overseas, strategically bought dozens of medical supply companies located across the United States. They then rapidly submitted $10.6 billion in fraudulent health care claims to Medicare for urinary catheters and other durable medical equipment by exploiting the stolen identities of over one million Americans spanning all 50 states and using their confidential medical information to submit the fraudulent claims. As alleged, the organization exploited the U.S. financial system by laundering the fraudulent proceeds and deploying a range of tactics to circumvent anti-money laundering controls to transfer funds into cryptocurrency and shell companies located abroad. The arrests announced today also include a banker who facilitated the money laundering of fraud proceeds on behalf of the organization through a U.S.-based bank.
The Health Care Fraud Unit’s Data Analytics Team and its partners detected the anomalous billing through proactive data analytics, and HHS-OIG and CMS successfully prevented the organization from receiving all but approximately $41 million of the approximately $4.45 billion that was scheduled to be paid by Medicare. HHS and CMS intend to seek to return the $4.41 billion in escrow to the Medicare trust fund for needed medical care. The scheme nonetheless resulted in payments of approximately $900 million from Medicare supplemental insurers. To date, law enforcement has seized approximately $27.7 million in fraud proceeds as part of Operation Gold Rush.
In another action involving foreign influence, charges were filed in the Northern District of Illinois against five defendants, including two owners and executives of Pakistani marketing organizations, in connection with a $703 million scheme in which Medicare beneficiaries’ identification numbers and other confidential health information were allegedly obtained through theft and deceptive marketing. The defendants allegedly used artificial intelligence to create fake recordings of Medicare beneficiaries purportedly consenting to receive certain products. According to court documents, the beneficiaries’ confidential information was then illegally sold to laboratories and durable medical equipment companies, which used this unlawfully obtained and fraudulently generated data to submit false claims to Medicare. Certain defendants controlled dozens of nominee-owned durable medical equipment companies and laboratories that allegedly submitted fraudulent claims for products and services the beneficiaries did not request, need, or receive. Certain defendants also allegedly conspired to conceal and launder the fraud proceeds from bank accounts they controlled in the United States to bank accounts overseas. In total, the defendants caused approximately $703 million in alleged fraudulent claims to Medicare and Medicare Advantage plans, which paid approximately $418 million on those claims. The government seized approximately $44.7 million from various bank accounts related to this case.
Finally, a defendant based in Pakistan and the United Arab Emirates who owned a billing company allegedly orchestrated a scheme to prey upon vulnerable individuals in need of addiction treatment by conspiring with treatment center owners to fraudulently bill Arizona Medicaid approximately $650 million for substance abuse treatment services. According to court documents, some of the services billed were never provided, while other services were provided at a level that was so substandard that it failed to serve any treatment purpose. As part of the conspiracy, treatment center owners allegedly paid illegal kickbacks in exchange for the referral of patients recruited from the homeless population and Native American reservations. The defendant received at least $25 million of ill-gotten Arizona Medicaid funds as a result of the conspiracy and is charged with a money laundering offense for his alleged use of those funds to purchase a $2.9 million home located on a golf estate in Dubai.
Fraudulent Wound Care
Charges were filed in the District of Arizona and the District of Nevada against seven defendants, including five medical professionals, in connection with approximately $1.1 billion in fraudulent claims to Medicare and other health care benefit programs for amniotic wound allografts. As alleged, certain defendants targeted vulnerable elderly patients, many of whom were receiving hospice care, and applied medically unnecessary amniotic allografts to these patients’ wounds. Many of the allografts allegedly were applied without coordination with the patients’ treating physicians, without proper treatment for infection, to superficial wounds that did not need this treatment, and to areas that far exceeded the size of the wound. Certain defendants allegedly received millions in illegal kickbacks from the fraudulent billing scheme.
Prescription Opioid Trafficking
74 defendants, including 44 licensed medical professionals, were charged across 58 cases in connection with the alleged illegal diversion of over 15 million pills of prescription opioids and other controlled substances. For example, five defendants associated with one Texas pharmacy were charged with the unlawful distribution of over 3 million opioid pills. As alleged, the defendants conspired to distribute massive quantities of oxycodone, hydrocodone, and carisoprodol, which were subsequently trafficked by street-level drug dealers, generating large profits for the defendants. This coordinated action is a continuation of the Health Care Fraud Unit’s systematic approach to stopping drug trafficking organizations and their pharmaceutical wholesale suppliers, which together have fueled an epidemic of prescription opioid abuse for nearly a decade.
DEA also announced today that in the last six months, DEA charged 93 administrative cases seeking the revocation of pharmacies, medical practitioners, and companies authority to handle and/or prescribe controlled substances.
Telemedicine and Genetic Testing Fraud
In today’s Takedown, 49 defendants were charged in connection with the submission of over $1.17 billion in allegedly fraudulent claims to Medicare resulting from telemedicine and genetic testing fraud schemes. For example, in the Southern District of Florida, prosecutors charged an owner of telemedicine and durable medical equipment companies with a $46 million scheme in which Medicare beneficiaries were allegedly targeted through deceptive telemarketing campaigns and then fraudulent claims were submitted to Medicare for durable medical equipment and genetic tests for these beneficiaries. The Department continues to focus on eliminating health care fraud schemes that depend on telemedicine, including schemes involving fraudulent claims for genetic testing, durable medical equipment, and COVID-19 tests.
Other Health Care Fraud Schemes
The other cases announced today charge an additional 170 defendants with various other health care fraud schemes involving over $1.84 billion in allegedly false and fraudulent claims to Medicare, Medicaid, and private insurance companies for diagnostic testing, medical visits, and treatments that were medically unnecessary, provided in connection with kickbacks and bribes, or never provided at all. For example, in the Western District of Tennessee, prosecutors charged three defendants, including business owners and a pharmacist, with a $28.7 million scheme to defraud the Federal Employees’ Compensation Fund by allegedly billing for medications for injured United States Postal Service employees that were never prescribed by a licensed practitioner and largely were not dispensed as claimed. And in the Western District of Washington and the Northern District of California, prosecutors charged medical providers with allegedly stealing fentanyl and hydrocodone, respectively, that was meant for the providers’ patients, including child patients in need of anesthesia.
The post DOJ Charges 324 in Largest Healthcare Fraud Takedown in U.S. History — $14.6 BILLION Scheme Involved 96 Doctors, Nurses, and Pharmacists Targeting Medicare and Medicaid appeared first on The Gateway Pundit.